What are T Cells?
There are many different types of immune cells and among them T Cells play an especially key role. T lymphocytes are derived from bone marrow-derived stem cells. After differentiation and development in the thymus, they are distributed to the immune organs and tissues of the whole body through lymphatic and blood circulation to exert immune function. T lymphocytes are fairly complex heterogeneous sub-populations that are constantly renewed in the body, as they can have different developmental stages or functions at the same time. Among them, Effector T cells (Te) have the function of releasing lymphokines, Cytotoxic T cells (Tc) have the function of killing target cells, and Memory T cells (Tm) have the role of memory-specific antigen stimulation. T lymphocytes can live in vivo for months to years. Memory cells survived longer. These T cells can fight cancer cells and viral infections. Th cells in these T cells, also known as CD4 + cells, are activated by reactions with polypeptide antigens presented by MHC II (major histocompatibility complex). MHC II is expressed on the surface of antigen presenting cells (APCs). Once activated, cytokines can be secreted to regulate or assist the immune response. Tc cells, also known as CD8 + acting cells, express CD8 on their surface. These cells can bind to antigen directly through MHC I.
What are Engineered Immune Effector Cells?
Engineered Immune Effector Cells (EIE) is a high-purity specific identification of immune cells that recognizes specific antigens in vitro by using the patient's own immune cells to stimulate specific antigens. EIE cells are made into an immune cell preparation with a kill-specific pathogen, which is after infused into the patient, thereby improving the body's immune response and achieving a cure for the disease. Applications include treatment of viruses, mold infections, and cancer.
How to engineer Immune Cells?
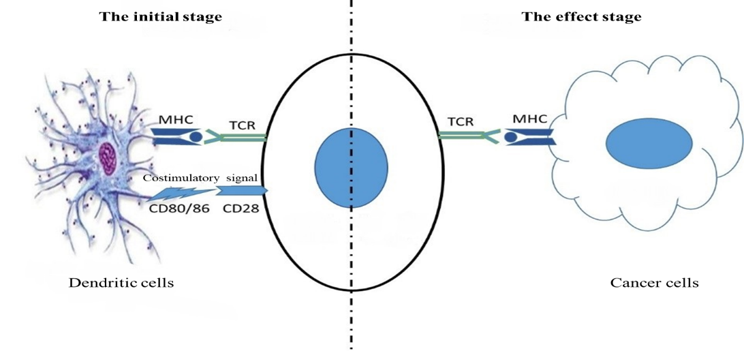
Two signals are required for specific immune T cell activation.
Signal 1: Antigen peptide-MHC molecular complex on antigen presenting cells binds to T cell receptor TCR specific recognition.
Signal 2: The interaction between T cells and many paired co-stimulatory molecules present on the surface of antigen presenting cells produces a costimulatory signal, of which CD28 binds to CD80/CD86.
First, lymphocytes and monocytes are isolated from peripheral blood mononuclear cells (PBMC), which induce monocytes to differentiate into high-efficiency dendritic cells (DCs). Then, they are subjected to specific antigens for lymphocytes. It is presented and cultured into a multi-functional immune cell population. The whole process can be completed in only two and a half weeks, it can be further expanded and used. Through the efficient antigen presentation and short-term preparation of DC, the cell collection and recovery can be shortened to 12-14 days for the process and clinical application of EIE.
In the aspect of EIE amplification, the cells can be restored to the number of lymphocytes originally co-cultured on the 7 to 10 days after co-culture (3 to 7 days, non-specific stimulation of lymphocytes will gradually become apoptosis), and the EIE cells can be collected for clinical use on day 12, and the rapid growth period on the day 12th-17th. At this time, according to individual differences, the EIE amplification is a multiple of 1 to 5.5 times, with an average of 2.04 times.
Personalized treatment
EIE therapy is tailor-made for each patient. The immune cells contain mixed specific immune cells such as CD4, CD8, NK, NKT. When the pathogen MHC molecules present antigen, EIE cells will be cleared after binding to pathogens, because each person's cancer cells are transformed from their normal cells, so the educated T cells can accurately kill the enemy without side effects. Moreover, with EIE therapy, the patient can still consider conventional treatments such as surgery, radiotherapy, and local chemotherapy. First, we let the cancer cells become weak, and then inject T cells into the tumor site. At this time, it is easy to stimulate the immune response and achieve the best therapeutic effect.